The U.S. emergency departments are struggling to cope with non-emergency visits that would have been prevented through timely and preventative transportation to a medical facility–particularly those at-risk patients experiencing complex mobility and weight problems. Bariatric patients are one of the most underserved when it comes to this category of people as they often need more special vehicles, specialized workers, and active care planning so that they can prevent the development of the situation to the state that would require them to visit an emergency room (ER).
This case study is an exemplary account of the long-term interaction of Infina Health with Mr. Samuel B., a 59-year-old male, with morbid obesity, congestive heart failure (CHF) and has limited mobility. Within six months, the bariatric transport team at Infina performed a series of preventative transfers, which enabled it to prevent over seven possible visits to the ER.
This was achieved by using a preventative approach, maintaining patience dignity, and logistical superiority according to Infina and this helped it reduce hospital load, decreased risks to the health of the patient, and enhanced the quality of his life all the same demonstrating the effectiveness of non-emergency medical transport (NEMT) as required ideally.
This case demonstrates why specialized medical transport is not a purely emergency enterprise but can be a component of proactive healthcare treatment. It also indicates a trend in the increased significance of bariatric transport programs as the number of individuals with problems connected with obesity keeps on increasing
2. Background/Clinical Needs on Patient
Patient Overview:
- Name: Samuel B.
- Age: 59 Weight 490 lbs
- Diagnoses: Morbid Obesity, CHF, DM Type2, HTN, CVI
- Living Accommodation: Assisted Living Facility (ALF)
- Physician: Nora Jefferson, Primary Care + Cardiology oversight
- Insurance: Covered in Medicaid Managed care + Secondary Long-Term Care Coverage
Clinical Needs:
Mr. B. was noted to have fluid retention history, as well as impaired mobility and ulceration on the lower extremities. Shortage of breath, chest tightness, and severe fatigue were weighting their occurrence and relied heavily on the absence of follow-ups in critical cardiology and wound care appointments because of transport lapses.
The ALF where he lived did not have personnel and even equipment to transfer him in a safe way, particularly when it is not an emergency. Previously 911 was inappropriately used when the patient had minor signs of distress causing overcrowding of ERs, providing unorganized care, and increasing the load on his insurance company.
Being aware of such patterns, Dr. Jefferson collaborated with Infina Health in developing a preventive care transport protocol; that prioritized:
- Timely visits by specialists
- Follow-ups in cardiology
- Wound dressing sessions every two weeks
- Regular diabetes examinations every month
- Non-dependency on ER-based emergency preparedness
The problem: how to move a high-risk bariatric patient safely, and without causing stress, injury, or embarrassment.
3. Problems Recognized
1. Difficulties of Transfer Connected with the Weight
A 61-year-old man (Mr. B.) living in Assisted Living Facility (ALF) weighed more than 475 pound. The following were found to be not just inefficient, but life-threatening as well: standard stretchers, gurneys and ambulance compartments.
He had previously had some very traumatic experiences of other services. He testified of how he almost fell in a rushed handoff and had to squeeze into spaces that could not fit his body. These experiences stamped him to use the words and phrases “humiliating” and “dehumanizing” to describe the process. His bulk was not merely logistical problem but required a man to show the sort of initiative that comes not out of the book.
The ALF did not have any form of bariatric lift piece, and the doorways were narrow, which added more risk and difficulty in transporting within the facility may be just as difficult as transporting outside of the facility. The team of Infina acknowledged that this is not only about the appropriate tools here, but also the right attitude which is required since all the members of the staff were to be competent in terms of both technical handling and person-centred approach.
2. Providers Gaps in Coordination:
One of the key problems was the disproportion of healthcare appointments made by Mr. B. and access to transportation. Some of his specialist visits were called off or postponed, frequently because of incompatible equipment or crews who were ill-prepared to handle his size, or his needs. Incurred delays caused a failure to attend wound care appointments, inability to treat edema, and blood sugar level management. Gradually he became less and less willing to cooperate with his treatment regimen. Such lapse of care eventually led to three ER visits over the past quarter, two of which would have been avoided with proper timely transportation and regular clinical check-ins. Inadequate coordination did not only affect his physical well-being but also destroyed his motivational levels and self-confidence.
3. Mental and Psychological Effect:
Mr. B. could not just be said to be having physical risks as he also had emotional scars. Any transport load led to the development of pre-trip anxiety and resistance. When being rolled along on the stretcher, he would keep on questioning staff, saying, “Does the stretcher have me this time?” and “Are they going to drop me again?” These were not mere phobias but founded on actual PTSD of the past and an ingrained sense of distrust towards medical staff and transportation. His failure to attend his appointments did not start out as an essentially logistical failure; they turned into a symbolic defence mechanism, the result of a long history of embarrassment, fear and self-perceived burden. His resistance to leave his room, even under the care of the in-facility care, highlighted some psychological injuries as a source of countering medical problems.
4. Facility Limitations:
There were few resources that were bariatric equipped; however, the Assisted Living Facility was otherwise well equipped to serve senior patients. The layout was compact; the beds and wheelchairs were of the normal size and the staff was not trained on how to provide mobility to the patient with morbid obesity. In the case of Mr. B. when he showed symptoms of congestive heart failure (CHF) that comprised shortness of breath, dizzy spells, and swelling, the facility did not have a system or mechanism to evaluate and de-escalate the problems. They called 911 even in the circumstances when it was stable, so that it could be treated with the help of oxygen or ordinary medical assistance. Not only these emergency calls were unnecessary, but they also stressed and disorientated Mr. B. and wasted the system with the unnecessary ER admissions.
5. Medical Complexity:
Making a transfer of Mr. B. was not an ordinary trip – it was a clinic on wheels. During each of his trips, his blood pressure, heart rate, and oxygen saturation levels needed to be measured in real-time, and he required low-flow oxygen support all the time. All travels were required to include a complete clearance by his own care doctor and the timing of the trips had to be compatible with medication requirements. Moreover, he could not sit upright long because of a backache and required a bariatric stretcher, which was reclined and pressure distributed. Lastly, all transport was to be pre-notified and coordinated with the receiving medical team, most specifically during wound care or cardiac review. The lack of any one of these factors could put him under great medical danger.
All of these five challenges were pointing in one direction to say that Mr. B. required much more than transportation, he needed a high-touch, clinically sound, and emotionally intelligent experience in care. Infina’s capacity to address these needs directly was crucial of turning crisis into continuity.
4. Transport Strategy and Execution at Infina
Having realized that Mr. B. situation was way more than only a pick-up-and-drop-off service, Infina Health introduced a multi-faceted, which had four levels of approach, a transport strategy that was more focused on the needs of bariatric patients with chronic medical conditions. It was aimed both at making sure that people were transported safely and with dignity and avoiding preventable Emergency Room visits by offering proactive, coordinated, and compassionate care.
A. Tailor-made Transport Planning
Infina Health also started every transport of Mr. B. with a 48-hour pre-trip care coordination protocol a structured method of planning that would not leave a single detail behind. The team did not approach each trip as a 1-time event; instead, the team considered every transport activity as a chain of care tied to the broader health outcomes of Mr. B.
Important actions were:
- Authority to verify the present weight and mobility requirements: Since the condition of Mr. B was changing, the care plan and the logistics of transportation had to change accordingly.
- Review of old clinical records: This assisted Infina to predict the presence of acute symptoms like Edema, hypoxia or wound infection that may hinder transportation process.
- Direct contact with the ALF and destination clinic: Infina communicated with sending and receiving facilities to ensure that the appointment times have been checked, access points to buildings, ramps or elevator availability, or extra hands required to help during a transfer.
- Medication and oxygen time coordination: The team coordinated prescription of medication to be used at the best time, as well as provision of maximum levels of oxygen during the whole travel and the period at the clinic.
These were not mere administrative planning activities; they were clinical safety netting, which ensured that Mr. B. would not be subjected to delays, mishaps, or other medical discomforts on the way.
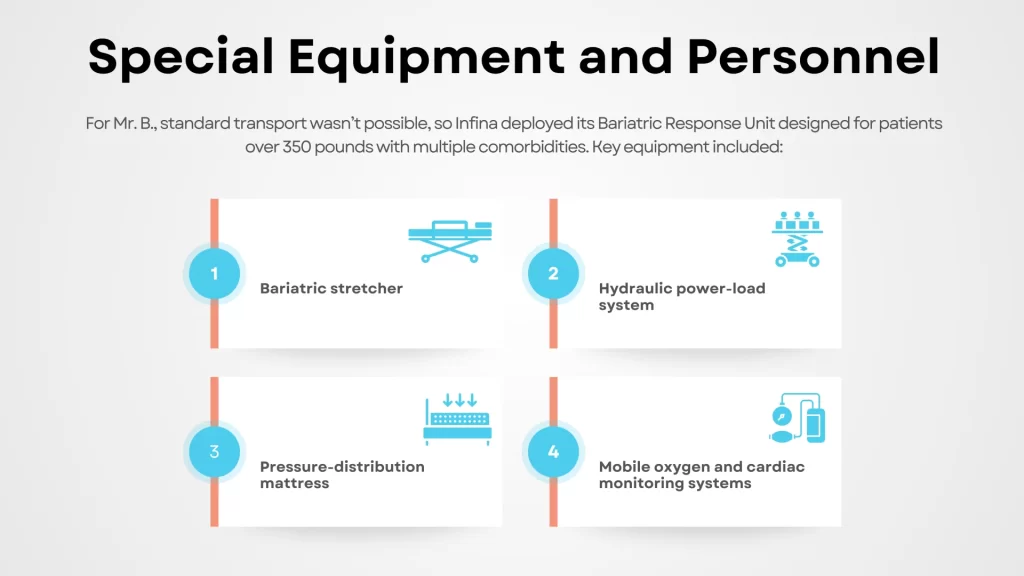
B. Special Equipment and Personnel
In the case of Mr. B. standard transport units were impossible. Infina used its Bariatric Response Unit that is specifically offered to patients exceeding 350 pounds, being diagnosed with two or more comorbidities and under medical supervision.
Important equipment was:
- Bariatric stretcher: Older, broader and longer with the ability to take weight up to 700 pounds safely and comfortably.
- Hydraulic power-load system: Prevented the necessity of employing manual lifting that could facilitate injuries to both the patient and staffs.
- Pressure-distribution mattress: It is imperative to prevent breakdown of the skin of Mr. B., especially in those areas likely to ulcerate.
- Mobile oxygen and cardiac monitoring systems: These allowed in-flight treatment and monitoring of the patient, particularly, during cardiac risk or respiratory drops.
The choice of the staff was also very strategic. All the crew members that served Mr. B. had been:
- Bariatric patient handling such as proper body mechanics and weight distribution and transfer methods.
- CHF (Congestive Heart Failure) symptom escalation protocol training, so they would know when to pay attention in situations that are threats before they happen.
- Trauma-informed briefings to work on language and tone patterns to use with Mr. B. language and tone that reflected respect of his lived experiences of anxiety, fear, and mistrust.
- Education on how to deal with bariatric related anxiety, like not using words like too big, heavy load and instead use words that indicated ability, safety, and respect.
These humanistic practices laid the foundation of regaining the trust that Mr. B. placed in medical transport.
C. Psychological Comfort/Routine Familiarity
Infina realized that the anxiety of Mr. B. was not an add-on, it was a clinical element. To deal with this, the crew was purposedly made to develop emotional continuity, which involved keeping the crew members together as much as possible.
This continuity was a success. Mr. B. started to know his EMTs by their faces, remembering their names and eventually letting them know that he was afraid. Each visit resulted in a relational rather than transactional dynamic. His preset tension was cut down a notch as he was able to see known, understanding staff at his front door.
Comfort measures involved:
- Verbal reassurance during the loading, travelling and unloading periods.
- Empowerment, or teaching Mr. B. to use a signal to show that he was OK without panicking.
- Taking Mr. B. into the process, detailing every step of the loading and equipment setting up process where he can feel heard and important.
- That was done after the trip where the EMTs would request feedback like, how did that feel today, and was there anything we could have done to make you feel more comfortable?
Such a strategy did not only pursue a lower level of psychological distress but also improved physical results. Mr. B. used less heart rate and blood pressure spikes in the transportation due to anxiety decreased.
D. Continuous Data Gathering
Infina, to achieve accountability and constant improvement, introduced a real-time Bariatric Transport Tracker that would record clinical and experiential data points following each transport.
Some of the measures followed were:
- Response time and trip length
- Blood pressure, oxygen saturation, and heart rate are vital signs in transport.
- Performance of equipment including tilt angles of stretchers and output of oxygen tanks
- Comfort indicators such as the ulcer-prone pressure point checks and the patient-reported discomfort
- Satisfaction scores of giving clinic personnel, ALF nurses, and Mr. B. himself
This data has not only been archived but was in fact reviewed by the transport leadership and medical advisory team of Infina, on a weekly basis. When on an entry, Mr. B. reported he had a sense of “slight dizziness” when transferring up inclines, the team changed the level of the stretchers and included a wedge underneath. When he complained that he felt rushed when unloading, Infina Health team added more time to the ends of the trip.
Through this responsive feedback loop, Infina managed to record a perfect safety record in 18 trips in a row. Not a single appointment was missed and there were no emergency interventions in transit with none of the patients going to ER in the quarter since the implementation of the transport strategy.
5. Results & Measurable Outcomes
Medical Impact
During a period of six months, Mr. B. had no emergency room visits, which was a significant improvement since, during the three last quarters, he had had to visit the ER three times. This drastic change was greatly attributed to the preventive, timely transports that never failed to make him receive cardiology, wound care, and nutrition visits.
The healing of his chronic wounds was accelerated because he fully complied with the dressing changes and debridement in a clinic. Most clinicians noted that there was less tissue inflammation and improved circulation during the initial eight weeks.
After periodic cardiology assessment and adjustment of medications in time, his CHF symptoms remained consistent. Fluid retention was checked effectively, and it was countered before it became critical. Interestingly, he did not readmission himself at all which used to happen once per month before.
Furthermore, the regular vitals recorded in transit could enable experts to monitor the early indicators remotely, which added to the overall disease management protocol of the patient.
Patient Impact
Mr. B. became significantly more involved in his personal care path. In subsequent surveys that the patient relations team of Infina administered, he gave 9.8 (out of 10) in overall transport experience, citing comfort, dignity, emotional support, as the crucial elements.
He stated, “I feel like I am part of something that is working on me and not just on me.”
After two months, his rate of keeping appointment shifted to 100%. His psychological and emotional well-being also improved, reducing the number of anxiety pre-travel attacks, and significantly reduces cooperative behaviour during care.
The Provider/Facility Impact
The Assisted Living Facility (ALF) Mr. B. lived in got a good boost, as well. Citing a huge decrease in emergency 911 calls, the staff noted that Infina scheduled transport was a trusted option where their semi-urgent needs were concerned.
Internal caregivers at the ALF had reduced physical and emotional stress, as they were no longer needed to assist manually or to “get by” with improper fitting transport aids.
Providers in the destination clinics observed increased compliances on the part of Mr. B. he adhered to dietary regimens, accepted changes in medication and was quite active in communication with his doctors. This enabled doctors to engage in effective care planning, without having to worry that the patient would not comply.
Communication with the external medical teams and Infina became frictionless and less complicated. Receiving facilities would be able to plan, allocate proper resources and provide better clinical care in an efficient manner.
Infina Health Outcome Indicators
Strategically, the case helped Infina Health create a new classification of service Preventive Bariatric Transport. The team designed an elaborate internal playbook, including best practices, equipment usage, psychological support practices, and data-capturing procedures.
This initiative resulted in an upsurge of the referrals of scheduled bariatric transport by 31 percent in two quarters. Facilities and providers also started referring to Infina in more specific situations requiring emotional care that was at least as important as the physical attention patients received.
The financial impact for Infina was also favourable because the reimbursement rates improved, the payers and case managers started to appreciate the proactive approach to transport as a method of decreasing emergency visits, admissions, and complications related to inpatient stays.
Such a better revenue cycle allowed the investing back in specialized equipment and training as well. Notably, the Bariatric Preventive Program developed by Infina was considered by one of the regional Managed Care Organization (MCO) as the model of excellence. This credit paved the way to new contracts and made Infina an exemplary mobility support provider to the mobility-challenged populations.
Lessons Learned and Strategic Takeaways
1. Healing the Bariatric Needs Humane-Competence
The half of the equation is the physical accommodations alone. Being aware of the emotional stimuli of bariatric patients and meeting them in advance creates loyalty that increases compliance with care.
2. Thousands Can Be Saved by Prevention Transport
Avoided ER visits saved money at a rate of about $1,800 to 2,200 per ER visit at a system-wide level. Preventive NEMT used on a large scale is capable of changing both organizational efficiency and the health of patients.
3. Continuity Is Everything
The fact that they were using the same transport crew to most of the trips brought in the caring relationship and steady relationship. Having known the patient and his cues and fears, supportive interventions were possible.
4. Partnership with Providers Is Necessary
Infina managed to provide an efficient process to deliver consistent results through the shared channel of communication with Mr. B. and his care team. Pre- and post-trip coordination eliminated care lapses.
5. Document Everything the Bariatric
Tracker tool provided Infina with real-time performance, patient satisfaction, and early warning indicators- eliminating negativity and improving the future planning.
7. Conclusion
The case study demonstrates that preventive medical transportation is not an optional feature: it is a safety necessity of high-risk groups of patients, such as bariatric patients. Infina Health has this holistic philosophy of being clinically prepared, operationally sensitive to the person, and being strategically ahead of the time, which allowed the proper attention to Mr. B. without using emergency rooms on a regular basis.
With the increasing need in complex transport, infina can be distinguished not by a right number of vehicles or tools, but by developing the system that brings the values of dignity and prevention to the centre of care delivery. Not only is this model replicable but imperative to future-ready healthcare systems that focus on outcomes more than reactions.