1. Executive Summary
Ms. Aisha M. was a 68-year-old woman resident of rural Worcestershire, who had to undertake significant difficulties in managing Type II diabetes, stage 5 chronic kidney disease, and limited mobility because of neuropathy changes. Going to her closest dialysis facility in Birmingham, a journey of almost 90 miles, daily 3 days a week became increasingly difficult not only physically but also emotionally. Fluid overloads, high costs of care provision, lack of quality life occurred because of missed sessions.
Infina Health came in with a planned care-coordinated transport strategy that provided consistent care transport services when it comes to dialysis transport services that matched her clinical and psychological needs. During the course of more than half a year, Infina allowed attending 72 dialysis sessions by its client with a guaranteed 100 percent session attendance, stable clinical indicators, as well as a marked improvement of emotional well-being. Still, it is worth noting the fact that Ms. M. no longer experienced as many hypoglycaemic episodes as possible, Edema decreased, and she felt independent.
Infina integrated route efficiency, trained transport staff, and patient-centred communication with in-transit vital monitoring and transformed transport into an active part of clinical care. Medical transport can create links to healthcare access and patient adherence, which is possible to see on this case with regard to medically complex groups of patients. It also demonstrates the importance of preventive, routine transport and management of chronic diseases.
2. Medical Background and Clinical Setting
Patient Profile:
- Name: Aisha M.
- Age: 68
- Conditions: Type II diabetic with neuropathy, stage 5 CKD on haemodialysis thrice a week, hypertension and diabetic retinopathy
- Mobility Level: Has difficulty walking more than 20m, frequent episodes of orthostatic hypotension.
Healthcare Setting:
Ms. M. lived in a small town in the countryside with poor transport providing the city with access. Her nearest dialysis centre was 45 miles distant. The transport was tedious and tiring, and her transport was frequently delayed or cancelled due to poor weather resulting in a missed session. It led to fluid retention, hypertension crisis, and emergency visits.
Effect of Non-Attendance of Sessions:
Each missed dialysis appointment presented an immediate risk: elevated potassium levels, water retention, high blood pressure and subsequent periods of emergency treatment. Ms. M. was subject to three emergency transports in three months (transport cancelled or delayed): two times because of fluid overload, once because of severe hypoglycaemia caused by missed meal prior to session.
Social and Emotional Effect:
The fear of transportation had a horrible effect on her emotions. She cited anticipatory dread in the presence of travel days, the fear of falls during transfer, and frustration of dependence. This greatly decreased her eating habits, sleeping and participation in personal care routine.
Healthcare Coordination:
Her doctor (nephrologist), Dr. Kumar, made an urgent referral to a stable means of transport that would secure her treatment appointments. Before the next session, her primary care team collaborated with Infina Health to set a regularized and weekly transport protocol, including pre- and post-session vital checks and personalized help during boarding.
3. Identification of Challenges
The intervention process of the case of Ms. M., a 66-year-old diabetic patient with end-stage renal disease, initiated with the identification of the barriers that previously long interfered with her life continuity and the quality of life. Based on the assessment of her care team, transport coordinators, and social workers, five very problematic areas of challenges were uncovered and will have to be strategically resolved.
A. Geographic and environmental barriers
The dialysis centre was more than 30 miles away in a rural environment where Ms. M. lived in an underserved location. The topography involved filthy roads, lots of snow during winter seasons and small gravel tracks, which were quite impassable during rainy days or freeze. Such environmental conditions did not only create problems in the transport timetabling but also put immense pressure on regular cars.
The informality in the majority of local transportation was caused by the remoteness of the area, as either cabs without any medical background came to the rescue or networks of volunteers who were not ready to take people who needed help with oxygen tanks, diabetic foot protection, or questions of instability. Missing, tardiness, and breakdowns were a popular way of life. Such variations jeopardize her compliance to dialysis regularly.
B. Compliance and Medical Complexity Risk
Treating a diabetic patient with dialysis is a special risk, particularly with regard to fluid crossovers, glucose, and potassium. A single missed dialysis session may lead to fluid imbalance, electrolyte imbalance or cardiovascular diseases. Ms. M. was also at risk due to the unpredictable pre-appointment practices. She also could risk and become hypoglycaemic during transportation or during her dialysis sessions unless she had eaten right or had injected her insulin under supervision.
The earlier providers did not check on such preconditions prior to pick up. On another occasion, she fainted during the trip and was taken to the ER because of low blood sugar but pre-transport monitoring would have eliminated that issue. Her chart was marked with several instances of the label of non-compliance, but not because the patient refused, but because there were holes in the planning of transportation and clinical context.
C. Mobility and Neuropathy
Ms. M. had peripheral neuropathy of progressed degree, and it resulted in a diminished feeling in her feet and legs. This made her walk shorter distances and footings quite difficult and, in many cases, the need to be assisted. Nonetheless, in the past, inconsistent or untrained escort support caused fall incidents such as head injury when she was trying to transfer out of a van into the ramp of the dialysis facility clinic entrance.
She had equipment (a rolling walker and protective leg wraps) which was frequently either lost or put on carelessly. These mobility risks not only rendered transport to be stressful but dangerous.
D. Inefficient Communication Infrastructure
There was a virtually non-existent coordination between the transport provider to Ms. M., dialysis team and home nurse prior to the intervention of Infina. She was often informed about transport delays or cancellation only an hour or two before she was supposed to be picked up. It lacked a centralized system where the appointment could be rescheduled, or her insulin or hydration plan could be corrected. Her care team could not communicate real-time information with drivers of the transport on the issue of urgent medical precautions, like unstable glucose readings or recent infections.
This discontinuous communication led to frequent failure of continuity of care.
E. Emotional and Psychological Obstacles
Fear of not knowing, rescheduling appointments, being considered an afterthought had worn Ms. M. out emotionally. She noted severe nervousness on each transport day that commenced hours prior to the pickup. The fear of being forgotten, showing up late and being turned down or falling with no one around was the worst to her. This emotional stress tended to make her skip dialysis appointments as a whole in panic or exhaustion.
She called it “a spinning wheel of stress.” The emotional burden concerned her daughter, who was traveling three hours to see her, as that was speeding up the deterioration more than the disease. Ms. M. was starting to cut herself off, to lose trust, and accept that care gaps were normal, until Infina entered the picture.

4. Infina Transport Strategy and Execution
The staff at Infina Health realized that they had to do more than provide a transport service to a dialysis patient to and from her medical appointment when Ms. M. was referred to the company dialysis transport program. A clinical-level, emotionally sensitive, logistically uniform system that does not only take her point A to B and leave was what she required, as it would guarantee her safe, enjoyable, and stable ride throughout. Infina employed multi-layered transport strategy that draws a combination of personalized scheduling, onboard safety, emotional support, and integrated care communication.
A. Specialized Logistics and Communication
Infina received its problem-solving skill by rearranging the planning of Ms. M. weekly transport to provide her with certainty and serenity. The transport coordinators implemented the 48-hour coordination call pre trip, during which Ms. M. or her caregiver would establish whether she was ready to go, whether it was safe outside (weather, road conditions), whether her home access points (ramp, steps, gate, etc.) were safe to load her. This basic check lowered last minute withdraws and crews arrived ready with the right gear (ice grips in snow season or walker support in rainy days).
Rather than making ad-hoc arrangements, Infina established regular weekly schedules to transport Ms. M. dialysis days were not ad-hoc and they came with specific pick and drop times which were informed to her family beforehand. This minimized her apprehension of transportation.
Furthermore, 24/7 direct contact line was established between Ms. M. and her daughter. In case of an alteration of her clinical status or a desire to know a bit about the ETA of the crew, there was always a person who could answer such questions–a practice that created confidence and empowered them.
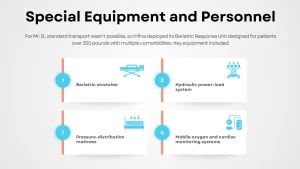
B. Special Transport Crew and Equipment
One of the most important shifts in the care of Ms. M. was the appointment of a Mobility-Assured Escort, or a trained assistant, who would have assisted her in walking out of the home and into the vehicle, and, on the way, into the ramp safely and into the transport seat. This assistant also made sure that her rolling walker as well as personal medical supplies were loaded accordingly.
The medical comfort apparatus involved in the vehicle was specially equipped by a non-slip floor, a wheelchair accessible lift, side stabilizers, a reclining seat with additional padding, and a compact hydration kit. This was not the norm in past rides where she used to come dehydrated, nervous and physically unstable.
Significantly, essential surveillance equipment was mounted on board. Transport team monitored and recorded her blood pressure, pulse, and oxygen saturation (SpO 2) both before and after each ride. This data was recorded as part of a transport log and reported back to her dialysis facility and had great value in pre-treatment hydration (or early identification of clinical distress).
C. Psychological Safety and Power
Infina understood that Ms. M. also needed emotional security, as much as physical safety. The plan entailed the provision of a transport crew that she knew well and had established rapport and trust with. She felt visible, looked after, and less like a just another pickup when she saw the same faces on Tuesdays and Fridays.
The staff were taught trauma-informed communication. The entire transport process was discussed in a very soothing tone starting with loading and route updates. Simple statements of such as now we are taking up your wheelchair, or in 10 minutes we shall be there and you may relax, are effective statements which emanate power in reducing fear and establishing a calm relaxing atmosphere.
To further ease her anxious nature with regards to transport, the crew played soft background music and provided light conversational moments and most important, observed her quiet times when she wanted it. These non-clinical gestures made a deep therapeutic effect to her confidence and involvement into care.
D. Clinical feedback loop
Infina did much more than transferring moms, it created a bridge between Ms. M. (home), the dialysis clinic, and her transportation crew. Each trip produced a Transport Log, with vitals, changes encountered on route, feedback of Ms. M., and environmental factors (e.g. whether the route felt especially bumpy, or whether she appeared pale or lethargic).
The transport coordinator discussed this information weekly with Dr. Kumar (her nephrologist) and the dialysis nursing staff. Following this feedback, the clinic made some minor yet important changes in the care of Ms. M., i.e., adjusting her fluid elimination goal or changing the start time of the sessions in order not to stress about the traffic.
The protocol also included emergency escalation. In case her vitals were not within safe limits or Ms. M. gave an impression of being cognitively impaired or excessively tired, the transport cadre informed its clinic or the nephrology helpline. This active surveillance eliminated ER visits that could otherwise have happened due to undetected symptoms or transport associated distress.
In this way, Infina offered a transport service that was much more than an ability to transport a patient; it would be a vital component in her care continuum.
5. Results and Measurable Outcomes
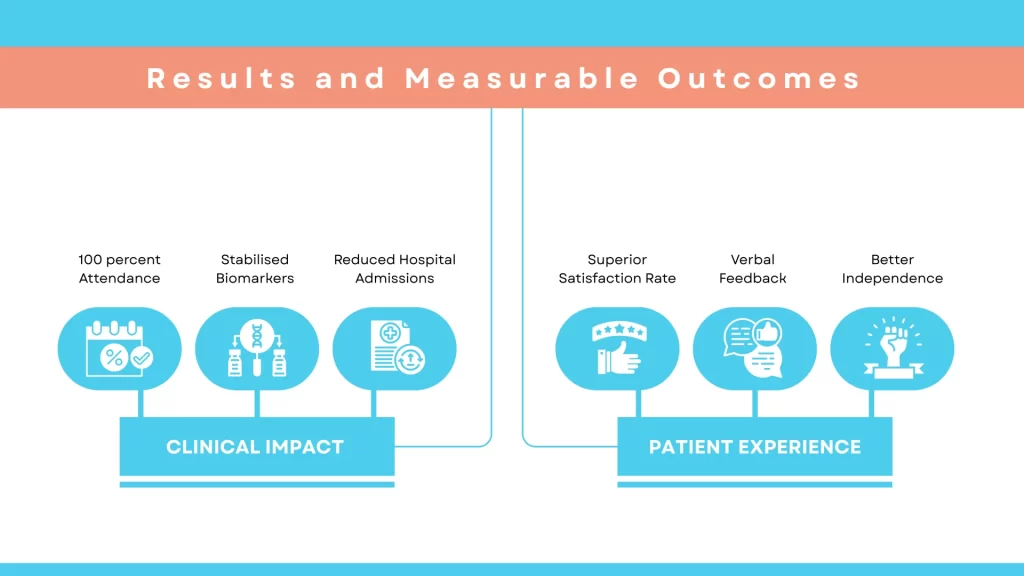
Clinical Impact
- 100 percent Attendance: M. attended every scheduled dialysis treatment (72 of them through) in six months.
- Stabilised Biomarkers: Potassium, urea, creatinine levels did not exceed the permissible range; the presence of fluid retention decreased by 80%.
- Reduced Hospital Admissions: Four Nights in ER: hypoglycaemia caused by dietary mistake but not connected with transportation.
Patient Experience
- Superior Satisfaction Rate: M. rated the transport service with 9.6/10 in the satisfaction surveys.
- Verbal Feedback: “I am safe”, she said. “I am dreading the travel days no more, like I did in years.”
- Better Independence: fewer fears, busier activities, no more distancing, she does her mini-walks and restores her hobbies.
Provider and Facility Impact
- Clinic Feedback: Dialysis nurses mentioned that the patient offloading process was much smoother since transport logs indicated a regular pre-session vital.
- Primary Care Report: Kumar viewed improved control of glycemia and reduced urgent changes into the medication.
- Efficiency in Coordination: The local practice learned to understand dialysis centres and Infina much better to eliminate rescheduling at the last minute.
Operational Metrics
- Referral Growth: Infina saw a 27 percent rise of rural dialysis transport requests in local clinics.
- Service Model Validation: Health commissioners awarded the model as a patient-oriented and cost-friendly model.
- Cost Savings: Prevented an estimated 1,200 hospital costs, and emergency procedures resulting in one missed hospital session.
6. Lesson Learned and Strategic Takeaways
- Trustworthy Transport Enhances Compliance: Predictability and frequent occurrence in transport is a must to compliance to chronic care.
- Mobility Support Eliminates Injury: Escorts could be trained, and suitable vehicles could reduce the number of trips, falls, and the fear of falling.
- Data Source: Transport: Data collected during their routine life-saving assessment by seafarers during transport would be useable clinical information.
- Emotional Support Boosts Clinical Alleviation: Crew empathy, having someone recognizable, and assuring them are also the key to attendance and feeling better.
- Collaboration is Key: Cross-stakeholder communication in real time between transport, clinic and primary care is a must.
Conclusion
Infina Health revolutionized how Ms. M. received her dialysis care by changing the orientation of transport as a way of preventing health challenges- not an afterthought process. The comprehensive strategy increased medical stability, lessened the number of acute hospital admissions, and spectacularly boosted her quality of life.
Such models are important as chronic diseases increase prevalence particularly in the rural and aging populations. The transport program run by Infina proves that health systems can utilize patient-centred clinically knowledgeable transport services to cut down unnecessary hospitalization and empower patients.