1. Introduction
In the field of emergency medical transport, behavioural health patients are typically trapped in a grey area – they are medically stable, yet emotionally frail, mentally distraught yet not in immediate peril. To most of the ambulance providers, such situations are handled using the standard protocols. However, when a behavioural health patient walking through the multicultural care centre doors at Infina Health, they expect something on the level of both safe, medically sound care, as well as emotionally sound care.
This case study will trace the care crisis-sensitive and trauma-informed given to the person known as Mr. J, a 32-year-old male who was in the middle of an active mental health crisis with marked anxiety, dissociation and psychotic episodes by the Basic Life Support (BLS) unit of Infina Health. Mr. J needed non-emergent transport to a temporary shelter to a special ambulatory-based mental health facility within a 10-day period of observation. The method required more than wheels and sirens, it required emotional intelligence, clinical restraint, cultural sensitivity, and a psychological approach in transport protocol.
The BLS technique in behavioural health developed by Infina had as its guiding principle the fact that security and dignity are not mutually exclusive. Whether that is selecting adequate individuals and language to be used, altering the environment of the ambulance, and working alongside mental health professionals, everything was reorganized to turn it into a therapy experience as opposed to a triggering one.
It turned out not just to be a successful cycle of transports but also to provide a better understanding of how mental health patients react when they are not approached in a hurry but with understanding looks. Mr. J is a success story of traveling full 8 round trips without sedation, physical restraint, and without experiencing any event post interference by Infina through the application on the environment of the Behavioural Health-first BLS approach.
2. Patient Background and Medical Overview
Patient Overview
- Name: Julian P.
- Age: 32
- Place: Suburban Pennsylvania
- Principal Coding: Schizoaffective Disorder, Bipolar type
- Secondary Diagnoses: Hypertension, Mild Obesity (BMI: 31.2)
- Transport Requirement: Non-emergency psychiatric transport covered at behavioural health facility to be evaluated and get medication management.
The patient Mr. J. is a 32-year-old male whose behavioural health history is complicated; at the moment, he was released into a transitional housing program in the short-term after he was discovered to be talking to himself and disoriented in a city park. He had schizoaffective disorder, generalized anxiety disorder, and PTSD, and he had auditory hallucination, paranoia, and a panic attack.
He was an easy trigger and cooperative especially when he was provoked by uniform, sirens, or sudden communication. Although his condition did not command the experience of an involuntary hospitalization, his psychiatrist established that he required outpatient behavioral health care on the daily basis, medication supervision, and social service guidance within the subsequent 10 days. Yet, Mr. J did not have a stable mode of transportation and was disoriented, so he was at risk of missing appointments and going to the emergency room.
There were several risk indicators identified in the transitional shelter:
- Fluctuations in mood of agitation, in particular at transition points
- Failure to get into typical ambulance or ride-sharing cars
- Language reminder towards past experiences of incarceration
- Little acceptance of waiting long or inexplicable alteration of routine
Infina Health was summoned not merely to transfer Mr. J. and drop him down at the care facility, but also to act as a stabilizing impetus between his shaky home base and the facility. It was judged that a BLS-level response was appropriate, since he was medically stable, and this stability was dependent on emotional containment, and environmental control.
3. Identified Challenges
Following were the challenges identified in MR. J.’s case:
A. Emotional Lability with the Change in Stages
Mr. J. had an exaggerated startling response to environmental changes. Past experiences of moving him on regular automobiles came with loss of bearings and panic attacks in the middle of the trip. Even a brief period of wait on the curb side may lead to pacing, yelling or refusal to board.
B. Traumatic Experience with Hierarchies
Frequently he would relate EMT uniforms with arrest detective or involuntary admission to mental institutions. The sirens or dictatorial orders were the reminders of being hemmed in the past. This affiliation evoked a fight or flight response when one was being approached by someone dressed up in professional garb, regardless of how non-aggressive they appeared.
C. Disruption in Communication
Mr. J experienced hallucination and confusion, which are among his psychotic symptoms. When he was talking to unseen persons or giving other questions based on reality as being confrontational, at times. This posed grave doubts on the conventional consent, teaching, or medical evaluation.
D. Bolt or Flight-Contrary Risk
On several occasions before the involvement of Infina, he ran away through the doors of the vehicle or resisted to sit in the seat after getting into it. This exposed both patient and transport personnel to unsafe, non-secure transport unless engagements strategies were in place.
E. Nonstandard Transport Protocol
Numerous medical transportation providers who were not in the emergency business did not fancy or were not properly equipped to tailor their provision to behavioural health cases. Physical stabilization training was introduced in the structure of stand-by-BLS teams, but they did not have the psychosocial training to de-escalate or engage mentally ill patients in a trauma-informed manner.
F. An Eco sensitive Trigger
Visual clues such as bright lights, white ambulances, and closed rooms made Mr. J even more stressed. No sensory-friendly mode of transport existed, and there was no one to improve on that other than taking care of the situation in their own way, and this is what Infina did by introducing an innovation within its own BLS platform.

4. Behavioral Health Transport Strategy
Infina has formulated a four-pronged plan to address the needs of Mr. J. by providing a trauma-informed, emotionally intelligent BLS transport intervention.
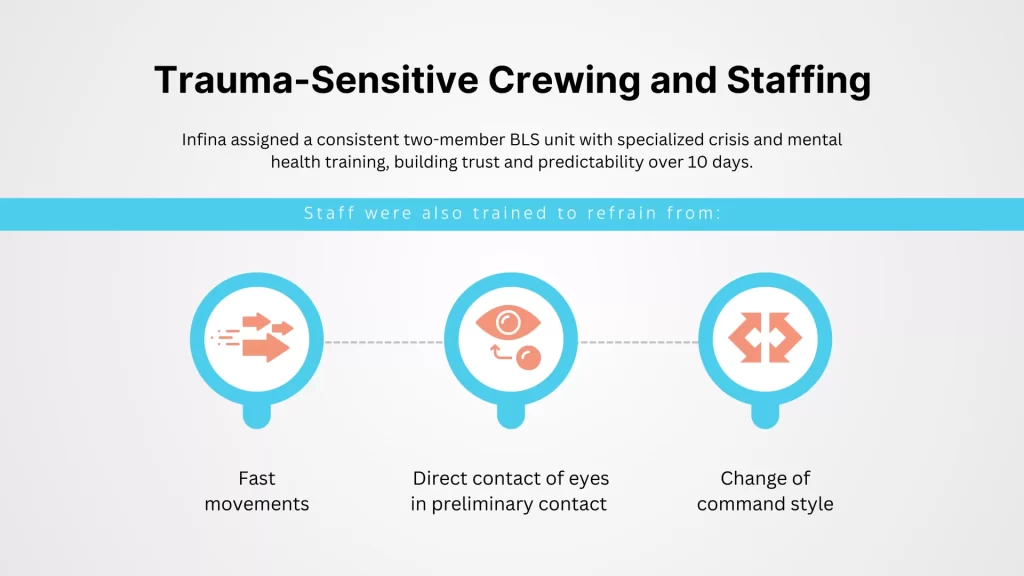
A. Trauma-Sensitive Crewing and Staffing
Infina picked a two-member BLS unit that underwent advanced behavioral de-escalation preparation. The lead EMT was a veteran of work in crisis stabilization units, and the partner EMT was a Mental Health First Aid certified EMT.
To minimize the fear presented by unpredictable personnel the entire 10-day period was covered by the same crew. This consistency enabled Mr. J. to come up with relational memory, which creates a foundation of trust and predictability.
Staff were also trained to refrain from:
- Fast movements
- Direct contact of eyes in preliminary contact
- Change of command style (e.g. “Get in the car” transformed to You are welcome to sit in our car now)
B. Unique Communication Technology
It was important to recognize the peculiarities of verbal and non-verbal patterns of Mr. J.
- Low Voices & Repetitive Affirmation: At the start of each ride, it started with the reasoning of “We are here to help. You are not in trouble.”
- Reality Anchoring: Useful phrases such as “Today is Tuesday; we are going to the clinic on Main Street” were used to establish oneself in the reality.
- Consent-Based Procedures: Consent-based procedures were followed in each action of opening the door, seat adjustment, belt securing, all announcements and verbal permission were followed.
This process cut-down the pre-trip anxiety of Mr. J. drastically after the 3rd ride.
C. Sensory-Modulated Ambulance Setting
Infina adapted the interior of the vehicle of Mr. J:
- Soft light rather than stiff LEDs overhead
- Reassuring blue covers bleaching white cabinets
- Soft music or ambient sounds that are played on a pre-approved playlist
- No sirens, no horn, and no loud radio talk
- Noise cancelling headphones were also provided and a lavender scented tranquilizing patch was placed within the vehicle.
The vehicle acted as a portable place to draw a breath and not a clinical box.
D. Transport Log and Cooperation in Mental Health
Infina developed a special Behavioral Health Transport log:
- The attitude of Mr. J. at the airport during check in and out
- Indicators of physiological states of distress (pulse, facial, eye)
- Pre and post session verbal expression
This log was distributed to his psychiatric team and case manager in his shelter on a daily basis. The 10-day observation period also served to show real-time alterations to dosages, stressor anticipation, and an overall course of therapeutic intervention raised by clinicians around his transportation experience.
5. Outcomes & Measurable Results
The results of the tailored behavioral health BLS transport that Infina had to offer were quick and immense. Attending to the emotional, clinical, and logistical needs of Mr. J., the team replaced a rather explosive and unpredictable experience of transport with the one of stability, safety, and faith. These are not only positive outcomes of good rides, but measurable clinical engagement, patient behavior and operational performance.
These findings extend the importance of trauma-informed care procedures in the emergency medical transport environment and forms a new benchmark of expected behavioral health instances in Infina and elsewhere.
A. 100% Appointment Attendance
Mr. J. went through his planned outpatient sessions remarkably, 10 visits, and 8 round trips without a single absence, an exemplary punctuality mark that has never been attained in his previous treatment history.
B. No Cases of Crisis or Escalation
Although there were several risk flags, Mr. J. did not need to be sedated, did not involve the police, or was physically restrained at any given moment. This was a 100% record of non-violence in the transport period that would be during the pilot period.
C. Emotional Re-Involvement with Care
On the 5th ride, Mr. J. started to initiate a conversation and make expressions of appreciation. He used childhood memories, expressed emotions, and used humor with EMTs as well which meant that he had emotional control and an ability to connect with people.
Mr. J Quote: “You guys do not treat me as a criminal. You merely treat me as a person who tries to get better.”
D. Advance Clinical
The psychiatrists observed a better mood stabilization and adherence to medication. The enhanced therapeutic response was also explained by the predictable and safe transportation experience that eliminated a significant anxiety factor.
E. Replicability of Operation
The leadership of Infina formalized the methods applied in the case of Mr. J. into a Behavorial Health Transport Playbook that will be followed by future patients with comparable requirements. This was the basis through which the company had its behavioural BLS pilot expansion at the beginning of the year 2025.
F. Cost Savings and Avoided Emergency
Use of the System On average, Mr. J. has experienced 4-6 emergency visits on a yearly basis in the last few years, being mostly related to transport refusals, missed appointments, or incidents of psychiatric emergencies in the middle of the transportation. The Infina pilot resulted in no ER diversions of patients, which represents a cost savings of an estimated 20,000+ of emergency care costs. Also, during the transport window, no police dispatching, involuntary holds, or days in the hospital boarding were needed.
G. Innovation in Patient-Centred Recognition
The behavioral health care center recognized the cooperation with Infina due to its model of transporting patients with trauma and the success Mr. J. showed in his progress during the quarterly review. Coordinated case review between Infina as well as the psychiatrists of the clinic and the local health department was started to examine fringe associations. The case has become a part of provider training to be transported by mental health-appropriate means.
H. Bigger Impact
The community experienced some ripple effects as a result of Infina successfully executing this pilot. Behavioral health practitioners started referring other patients to receive specialized BLS transportation. It was also the driver to discuss with state Medicaid partners behavioral transport as a preventive care service, as opposed to an emergency solution, as part of the reimbursable services.
Collectively, these results not only signify restored humanity in the experience of Mr. J., but it also suggests the scalability of a solution of humanized kindness in psychiatric transport across systems.
6. Long Term Impact and Strategic Value
The effectiveness of the behavioral BLS transport of Mr. J. spread much further than that of a patient. It exposed a crucial weakness in the logistics of mental healthcare and demonstrated that, even in a high-risk psychiatric population, stress-resistant mental health transportation is possible when it is trauma-focused. The members of the Infina team did not only provide safe patient transfers but introduced an example of integrating clinical intent and logistical performance.
The case proved that strategic modifications of Basic Life Support (BLS) transport may lead to significant changes in patient outcomes, system burden, and can precondition a provider to become a pioneer of behavioral health innovation.
A. Less Load on Emergencies
Prior to the intervention of Infina, the number of ER visits as a result of skipping appointments and making disturbances in the street was high in Mr. J. During a 30-day monitoring period following transportation, no emergency services were called (because of behavioural needs) that would have cost emergency responders time and money.
B. Optimization of the Value-Based Reimbursement
The reimbursement process with the Managed Medicaid provider who pays the costs of Mr. J.s care officially recognized the presented model of Infina as preventive transport with medical necessity, providing access to new funding opportunities previously available to acute care.
C. Pattern of Behavioral Health Justice Reform
Infina has spent a long time in promoting a broader movement of decriminalizing mental illness through its gentle transport model. Their solution demonstrated that it was possible to ensure safety without uniforms, sirens or force-an understanding that is in harmony with progressive ideas in public health and justice reformation.
D. Reputation Improvement among Community
Transitional housing programs and mental health facilities started sending their like-minded patients to Infina, as they heard a lot about their non-judgmental and patient-cantered attitude. The company was featured in its response to crisis in communities through the Best Way Practice, based on the company Behavioral Health Transport Program.
7. Conclusion
The BLS transport of Mr. J. by Infina Health was above whatever needed to be expected of such a non-emergency ambulance service. Instead of viewing a psychiatric patient as a logistical issue, they developed an answer that is based on dignity, understanding, and order.
- J. did not need sedation. He required some stability.
- He did not require being bound. He had to feel secure.
- Most importantly, he did not need to be dealt with. He had to be visible and nurtured.
The case demonstrates that the issue of behavioural health transport is not limited to transporting patients to or between facilities, but rather it is an aspect that should provide the continuum of compassion in one of the most vulnerable moments of the life of a person.
The field of Behavioral BLS, which Infina has spearheaded, is redefining safety-based medical transportation as trauma informed. With an increasing number of systems now ideally reconsidering the domain of mental health logistics in the context of a care-first sensibility, the protocol at Infina Health provides a critical roadmap of how to not just avoid emergency but make a beeline into opportunity, but also how to transport with the heart as well as the head.