How to Ensure Patient Safety and Care in Critical Care Transport
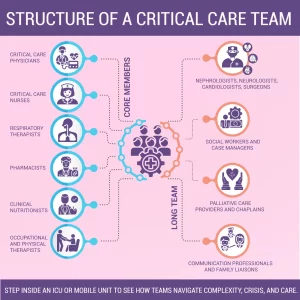
Critical care transport involves the safe and effective transfer of critically ill or injured patients between healthcare facilities. These patients often require advanced life support, constant monitoring, and intricate medical interventions. This complex process necessitates a multidisciplinary team of highly skilled healthcare professionals, including physicians, nurses, respiratory therapists, and paramedics.
In this blog, we will look into the essential elements of critical care transport and explore best practices and key strategies that healthcare providers, transport teams, and organizations can adopt to ensure optimal patient outcomes during these critical transfers. By understanding and implementing these protocols, medical professionals can significantly reduce risks and provide the highest level of care for patients in transit.

Critical care team of nurses, paramedics, and EMTs providing emergency medical assistance to a patient in an ambulance.
Types of Critical Care Transport
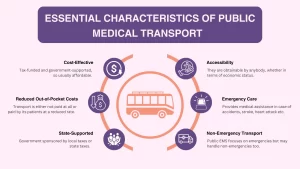
There are three primary modes of medical transport used for critical care transportation, each designed to cater to the specific needs of critically ill patients:
- Air Ambulances (Helicopters and Fixed-Wing Aircraft): Air ambulances are often used when time is a critical factor or when the distance between medical facilities is too great for ground transportation. Helicopters are typically employed for short to medium distances, especially in urban or rural areas, while fixed-wing aircraft are used for longer-range transports, including across states or countries.
- Ground Ambulances (ICU-equipped Vehicles): Ground-based transport is most common for shorter distances or when air transport isn’t feasible due to weather or other conditions. These ambulances are specially outfitted with advanced medical equipment, including ventilators, infusion pumps, and monitoring systems, to provide intensive care during transit.
- Interfacility Transport: This type of transport involves moving patients between healthcare facilities, such as from a local hospital to a specialized center with more advanced treatment capabilities. It’s often used for patients requiring specialized care, such as organ transplants, trauma surgery, or neonatal care.

Two medical transport professionals reviewing a patient’s medical records to ensure proper critical care transport service
Who Qualifies for Critical Care Transport?
Critical care transport is designed for patients in severe, life-threatening conditions who require continuous medical intervention and monitoring during transit. These patients often cannot be moved safely without specialized equipment and highly trained medical personnel. Some of the key patient types requiring a critical care ambulance include:
- Patients suffering from severe trauma, such as those involved in car accidents, falls, or violent incidents.
- Patients with organ failure (e.g., kidney, liver, or respiratory failure) often require transport to specialized facilities.
- Neonates, especially those born prematurely or with congenital conditions, require specialized pediatric intensive care units (ICUs) for transport.
- Time-sensitive conditions like strokes require quick intervention to minimize brain damage.
- Individuals experiencing acute cardiac events, such as heart attacks or arrhythmias.
Need reliable critical care transport for your patient? We provide state-of-the-art equipment to ensure the highest level of care during transit.
Risks and Challenges in Critical Care Transport
Transporting critically ill patients involves numerous challenges. Key risks in critical care transportation include:
1. Instability of Critical Patients
One of the primary risks is the instability of the patient. Critically ill individuals require continuous monitoring and interventions for vital functions like airway management, circulation, and breathing. Small changes in their condition can escalate quickly during transport, potentially leading to life-threatening complications. For example, a patient with severe trauma may need frequent blood pressure monitoring and fluid resuscitation, while a cardiac patient may require medication adjustments or defibrillation.
2. Environmental and Technical Factors
Transport vehicles, especially air ambulances, present several challenges:
- Limited Space: The confined space in transport vehicles can restrict medical staff’s ability to access the patient or equipment, hindering the ability to provide timely care.
- Noise and Vibration: In air transport, loud noise and vibrations can impair communication among team members and cause discomfort to the patient, potentially aggravating their condition.
- Weather and Altitude Conditions: Weather conditions and altitude changes can affect oxygen levels, making it more difficult to maintain proper ventilation and oxygenation, especially for patients with respiratory issues.
3. Medical Equipment Limitations
Medical equipment in transport vehicles may face limitations due to power constraints, malfunctions, or calibration issues, potentially compromising care. Portable devices like ventilators, infusion pumps, and monitoring systems must be reliable to function properly in a mobile environment.
4. Communication and Coordination Challenges
Clear communication between the transport team, receiving hospitals, and other parties is crucial. Any miscommunication can lead to delays or errors in patient care, affecting treatment plans and outcomes upon arrival.
Essential Elements for Safe Critical Care Transport
Below are the key elements that contribute to safe and effective critical care transport:
1. Proper Pre-Transport Assessment
The foundation for safe CCT transport begins before the patient even leaves the facility. A thorough pre-transport assessment ensures that both the patient and the transport team are fully prepared for the journey ahead.
- Before transport, a comprehensive assessment of the patient’s condition is essential. This includes reviewing vital signs, medical history, and any specific needs or risks that may affect the transport process.
- It is critical to ensure that all necessary medical equipment is ready and functioning properly before transport begins. This includes portable monitors, defibrillators, IV fluids, medications, and emergency kits.
- The transport team must be fully briefed and trained to handle the patient’s specific needs. This includes a detailed discussion of the patient’s condition, the expected interventions during transport, and the roles and responsibilities of each team member.
2. Patient Stabilization and Monitoring
Stabilizing the patient before and during transport is vital to minimizing the risks of deterioration.
- Prior to transport, the patient must be stabilized to the greatest extent possible. This includes securing the airway, providing adequate ventilation, and stabilizing circulation. Vital signs such as blood pressure, heart rate, and oxygen saturation should be monitored and maintained within normal ranges to ensure the patient is in an optimal state for transport.
- During transport, the patient should be continuously monitored using portable medical devices to track vital signs, including heart rate, blood pressure, and oxygen saturation.
- In addition to basic life support monitoring, advanced medical technologies such as portable ventilators, blood gas analyzers, and telemetry systems should be utilized to ensure real-time assessment of the patient’s condition. These technologies provide crucial data on respiratory and cardiovascular status, which helps guide interventions during transport.
3. Maintaining a Safe Transport Environment
A safe transport environment is essential to ensure that the patient’s condition does not worsen during transit.
- Proper positioning of the patient is crucial to prevent complications such as pressure sores, discomfort, or airway obstruction. The transport team must ensure that the patient is securely positioned, especially if the patient has undergone surgery or has multiple injuries that require specific postures to avoid exacerbating their condition.
- Maintaining an appropriate environment inside the transport vehicle is essential for patient safety. Temperature regulation should be carefully managed, as patients may be at risk for hypothermia or hyperthermia during transit.
- All equipment, medications, and the patient must be securely fastened to prevent movement that could cause harm during transit, especially in air transport, where turbulence may occur.
4. Effective Communication and Coordination
Effective communication ensures that all team members are aligned on the patient’s condition, care plan, and any potential changes during the transport.
- Communication before transport is key to ensuring that both the referring and receiving hospitals are prepared for the patient’s arrival. The transport team should receive detailed information on the patient’s condition, specific medical needs, and required equipment.
- Throughout the transport process, the transport team must remain in constant communication with the receiving hospital. This allows for real-time updates on the patient’s condition and any changes that may require adjustments to the care plan.
- Upon arrival at the receiving facility, a thorough handover of care must be conducted between the transport team and the receiving medical team. This handover should include detailed information on the patient’s condition, any interventions or changes in care made during transport, and any concerns the transport team has identified.
5. Specialized Training for Transport Providers
The success of a critical care ambulance relies not only on the right equipment but also on a well-trained, highly skilled transport team.
- Critical care transport teams must be proficient in trauma management, particularly in high-stress environments. Advanced Trauma Life Support (ATLS) certification equips providers with the knowledge and skills to assess and manage trauma patients efficiently, stabilizing them before and during transport.
- For patients experiencing cardiac emergencies such as heart attacks or arrhythmias, Advanced Cardiac Life Support (ACLS) training is essential. This certification teaches advanced techniques for managing patients in cardiac arrest or severe arrhythmias, including the use of defibrillators and administering medications.
- Transporting pediatric patients requires specialized knowledge due to the unique medical needs of children. Pediatric Advanced Life Support (PALS) training covers pediatric resuscitation, including airway management, drug dosages, and handling cardiac and respiratory emergencies in children.
- Neonatal Resuscitation Program (NRP) is vital for teams transporting neonates, especially premhttps://infinahealth.com/services/advance-life-support-transport-in-philadelphia/ature or critically ill infants. NRP training focuses on providing life-saving interventions for newborns, such as resuscitation techniques, stabilizing their condition, and handling birth-related emergencies.
Conclusion
Patient safety and optimal care during critical care transportation requires careful planning, skilled teams, and continuous monitoring. At Infina Health, we are committed to providing the safest and most efficient critical care transport, supported by experienced professionals and state-of-the-art equipment.
If you need reliable and safe critical care transport services, contact us to discuss how we can assist you.
Frequently Asked Questions (FAQs)
[faq_dropdown]